How to Treat Severe Laminitis in an Ambulatory SettingReprinted with permission from the American Association of Equine Practitioners. |
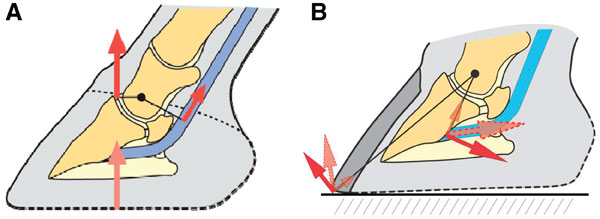 |
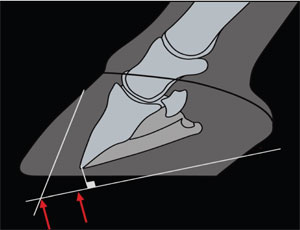
| Fig. 1. (A) Biomechanical forces (GRF, moments about the DIP joint, and force of the DDFT) exert on the equine foot at rest. (B) The GRT moves into the toe and the moment around the DIP joint at the beginning of breakover. |
3. The Mechanism
The anatomic structure of the tissues affected by laminitis has been well-documented. However, despite considerable advances in our understating of the pathophysiology of laminitis made over the two decades, there is still much to be learned about the initiating events and the pathways by which they lead to the clinical disease. The interdigitating dermal and epidermal lamellae and their related vasculature are positioned between the parietal surface of the distal phalanx and the rigid hoof capsule.The digital circulation to the proximal dorsal lamellae is through the coronary artery, and the distal dorsal lamellae receive their blood supply from branches of the terminal arch that form the circumflex artery. Any compromise or instability in the lamellae changes the position of the distal phalanx, which in turn, creates abnormal pressure on the vessels restricting circulation. The inflexible nature of the hoof capsule does not accommodate the inflammatory effects, especially edema, that occur in the laminar tissue during laminitis—this scenario could be considered a type of compartment syndrome effect.
Knowledge of the biomechanics and forces exerted on the structures of the foot, including the lamellae, is critical to the clinicians when formulating a plan to counteract these forces. Because the lamellae suspend the distal phalanx within the hoof capsule and accept weight, this structure is subjected to an array of mechanical forces. The main forces are the weight (load) of the animal, which is opposed by the ground reaction force (GRF) and the moments (a moment is the product of the length of a lever arm and the force perpendicular to the lever arm) about the distal interphalangeal (DIP) joint, in which the moment generated by the GRF is opposed by that load generated by tension in the deep digital flexor tendon (DDFT) (Fig. 1).4 These normal mechanical forces exerted on the foot become detrimental with laminar compromise. A laminitic horse that is painful will be reluctant to move, and when not recumbent, the horse's limbs will be approximately positioned as if in the mid-stance phase of the stride.The load (opposed by GRF) is located dorsal to the center of articulation and just behind and slightly medial to the apex of the frog on the ground surface of the foot.5 When the limb is loaded, the tensile forces in the DDFT create a moment, which unless opposed by an equal and opposite moment, causes rotation around the DIP joint. At breakover, the moment created by the DDF exceeds that created by the GRF. The tensions in the DDF are greater during the mid-stance phase of the stride than at rest, and they are further increased at the beginning of the breakover phase of the stride. The opposing moments generated by the GRF and the tension in the DDF lead to a distractive force within the dorsal lamellae. Dorsal capsular rotation is the most common form of displacement seen in laminitis, and it relates to the inability of the compromised lamellae to accept the load placed on the dorsal region of the foot during weight-bearing and breakover. Through the action of these moments and weightbearing,the lamellae in the dorsal area of the foot are under more tensile strain compared with the lamellae in the quarters and heels, which along with the frangible circulatory pattern in the dorsal section of the foot compared with the dual blood supply in the palmar/plantar area of the foot, predispose the dorsal lamellae to injury. The GRF determines the load and subsequent compressive and tensile stresses that are placed on the dorsal lamellae.The load or GRF on the foot cannot be changed, but the position of the GRF (center of pressure) on the ground surface of the foot can be shifted away from the affected area or redistributed. Support is a term that is widely used, seldom defined, and often ambiguous. Support usually means to hold a structure in place or prevent it from collapsing. In laminitis, it refers to supporting the distal phalanx and preventing it from displacing from its normal position within the hoof capsule. Attempting to counteract the weight of the horse by any physical means placed under the foot makes this concept of support unrealistic. The stresses on the lamellae are greatest during weight-bearing and locomotion, and an attempt can be made to redirect these forces by recruiting additional parts of the ground surface of the foot to bear weight to reduce the load on the lamellae. Decreasing the moment about the DIP joint reduces the stresses on the lamellae that are greatest during dorsiflexion of this joint. In a horse with acute laminitis, the already damaged lamellae have a greater propensity to separate with the stress associated during breakover. Shortening the toe decreases the length of the lever arm, and elevating the heels decreases the tension in the DDFT.
Finally, the sole needs to be considered. In barefoot horses with a good foot, the conformation and thickness of the sole is not only protective but functional,and it can be considered a weight-bearing structure. The sole in a shod horse has reduced functionality when it becomes suspended above the ground surface of the foot with shoes, plays a limited role in weight-bearing, lacks stimulation, loses sole depth, and is often subjected to inappropriate farriery. In the routine practice of farriery, one of the most common causes of lameness is excessive sole pressure in the presence of inadequate thickness or depth. There are a plethora of pads, devices, and materials on the market that are placed on the sole or under the horse's foot to counteract the weight in the early stage of laminitis. The rationale of this methodology of creating excess pressure on the ground surface of the foot in the face of insufficient sole depth has to be questioned. There are obvious limitations of applying physical devices to the foot: we are limited to a relatively small surface area in an attempt to offset profound vertical forces imposed on the digit, the sole has a specific thickness, and the application of pressure through compromised tissue may cause additional pain and tissue damage.5
4. Assembling the Team
The equine practitioner is responsible for addressing the overall health and welfare of the horse. When confronted with a serious case of laminitis, a farrier will also play a prominent role in treatment and in most cases of severe chronic laminitis, the predominant long-term role. The team is completed with the owner/trainer of the animal, who will often be the primary caregiver, the party who makes the decisions, and the person responsible for the financial obligations associated with the treatment. If either clinician (veterinarian or farrier) is inexperienced in treating laminitis, it is prudent to seek advice from or refer the case to an individual who is experienced and treats this disease on a regular basis. Current history, clinical impressions, and images can be transmitted from the farm to a referral center for a consultation. There are a multitude of methods/products available that all purport to improve the disease, but none are proven or even consistent. There are no controlled studies documenting the efficacy of any one medical or farriery procedure. Techniques change rapidly and for the most part, are empirical. Thus, laminitis treatment remains anecdotal and is based on the stage of the disease, clinical experience of the clinician, and response of the patient. Because there is no proven treatment that is superior to the other, dialogue is important between both clinicians, because there will be diverging thoughts, opinions, theories, and previous treatment experiences. The preferred approach may be to consider the individual case coupled with the radiographs and decide on a treatment strategy based on medical and biomechanical principles. When communicating with the owner, the treatment plan should always be presented in a consensual manner. The clinicians should present a unified approach to treatment, with neither party questioning the procedures of the other in front of the owner/trainer. Client communication is one of the most important but least discussed aspects of case management. A policy of open, honest communication that tempers false expectations of success must be used. Owners should be given realistic information from the onset: severe laminitis has a poor prognosis, there are no proven treatments, any treatment can be extensive, expensive, and prolonged, and treatment may result in euthanasia.1,5,6 Given the seriousness of severe laminitis, clients will likely look into other sources for information or hope such as the internet, horse magazines, and support groups regarding the management of their horse. It is imperative that the attending veterinarian and farrier are well-versed in the common inquiries that will arise and are able to address them prospectively. Accurately predicting the outcome of horses with laminitis is impossible. This lack of predictive power is understandable given the number of variables associated with management of severe laminitis, which includes not only the feet but the overall health of the patient in addition to client constraints. The owner must be warned that, if the horse with laminitis is insured, it is their responsibility to inform the insurance company immediately.
| ||||||||||
| Table 1. The Lameness Scale Developed by Obel Can Be Used to Document Laminitis Severity |
5. Assessment
Accurate assessment of the whole patient, with consideration for history, occupation, and owner expectations, should be considered in every case when attempting to provide appropriate treatment as well as prognosis. Diagnostics remain basic for laminitis, but thoroughness must be emphasized. A complete physical examination and in particular, detailed evaluations of the feet are mandatory. Assessment of the intensity of the digital pulse, temperature of the feet, and extent of lameness should be made. The coronary band should be assessed for the presence of edema, depressed areas that indicate distal displacement, and palpably tender areas that are associated with a possible abscess or separation of hoof wall. The shape and position of the sole is observed for degree of concavity or protrusion, soft spots, or excessive loss of depth. The size and conformation of the feet are especially important when designing a farriery plan for the horse and monitoring subtle changes associated with the progression of the disease. Hoof conformation may influence loading patterns and the type of displacement encountered. For example, in the author's experience, there will generally be more displacement in an upright or club foot because of the increased load on the dorsal lamellae caused by the pre-existing increased tension in the DDFT and corresponding dorsal center of pressure. Conversely, horses with a long-toe/low-heel conformation generally have thin soles, which limits the use of the sole in counteracting the weight of the horse.
In most instances, observation of the stance and gait provides a strong indication of the presence of laminitis. The characteristic stilted camped-out front legs are believed to redistribute load to the hind limbs.5 Variations in stance likely occur because of the presence of pain in the rear feet or variations in the location of pain in the front feet. It is not necessary to use local anesthesia to diagnose laminitis, and it should be avoided if possible.The Obel grading system for lameness in laminitis can be used to document the grade of laminitis and track the progression (Table 1).7
The clinician must determine the reason for and source of pain, its location, and the degree of instability (amount of pain) within the foot. The location of pain is important to determine from a therapeutic standpoint, because any pressure applied under this area in an attempt to support the hoof will exacerbate the pain. Hoof-tester evaluation is useful when positive, but a negative response does not rule out foot pain or laminitis. It is common to have a negative hoof-tester response in a horse with a thick sole and hoof capsule. Horses with metabolic syndrome also generally have a negative response. Hoof testers are also useful to assess the deformability of the sole, which gives a reasonable estimate of sole depth. Bilateral diffuse solar pain across the toe and dorsal wall is considered characteristic for laminitis; however, bilateral foot bruising may yield similar symptoms. Focal pain anywhere in the foot is generally associated with sepsis or abscess formation, but the horse may assume a laminitic gait to unload on the foot. Hoof wall collapse along the medial quarter and heel is another recognized entity associated with unilateral distal displacement of the distal phalanx. A marked hoof-tester response is often present in this area. It is not fully understood whether this is attributable to a greater degree of lamellar damage in this region or simply to regional mechanical overload on that section of the foot. Variations of the stance and gait are recognized when pain originates in areas other than the toe and dorsal wall. Laminitis involving the dorsal hoof will generally present with a heel-first landing, whereas a horse with palmar foot pain will present with a toe-first gait or flat-footed landing. It is not uncommon for laminitic horses to land toe first, possibly because the stride is so shortened that they cannot extend the digit or because it is a deliberate action to spread out the duration of loading the foot.
The most important determinant of prognosis in the acute laminitic patient, and one of the most difficult to access, is the degree of instability between the distal phalanx and hoof wall. At present, we have few, if any, means to make this assessment beyond the amount of pain, serial radiographs, thorough clinical evaluation, and response to therapy. In the first 48 h of laminitis, pain has been shown to correlate well with the degree of histological injury to the lamellae, making it a good predictor of instability.8
6. Acute Laminitis
When presented with a case of acute laminitis, three problems are encountered. First, there is no practical means to assess the extent of the laminar damage present and if this damage will be permanent when the animal first shows clinical signs of acute laminitis. The number of horses that suffer a severe laminitic episode that can be treated successfully after clinical signs are observed is also relatively small.3 The damage to the lamellae that occurs during the developmental stage of laminitis precedes the onset of pain and lameness noted in the acute stage. Second, there is no practical means to counteract the vertical load that is placed on the horse's feet. Stated differently, we have no practical device, product, or method that allows us to take the weight off the compromised lamellae. Third,the distractive force placed on the lamellae by the DDFT is also hard to counteract.
Medical Therapy
Laminitis often originates from an organ system remote from the foot, such as the gastrointestinal, respiratory, reproductive, or endocrine systems.Therefore, treatment during the acute stage needs to aggressively address the initiating cause of laminitis,or if treatment of the cause was initiated before the onset of clinical laminitis, it should be continued. Recently, unequivocal evidence confirms that an inflammatory response is present very early in the disease before other changes are present, suggesting that the vascular changes, thrombiformation, and metalloproteinase degradation of the basement membrane are downstream events.4 The main pharmacologic agents used to treat the inflammatory response in early laminitis are nonsteroidal anti-inflammatory drugs (NSAIDs). The analgesic effects of NSAIDs are important from a humane perspective but should be used judiciously so that the clinician is able to accurately monitor the clinical signs in the feet. Clinical improvement from the owners' perception is a decrease in pain; therefore, the clinician may be inclined to increase the dose of NSAIDs or combine NASIDs to appease the client. This practice should be avoided, because the analgesic effects of the NSAIDs will increase ambulation and place additional stresses on the compromised lamellae. The pharmacologic agents most frequently used to treat uncomplicated laminitis are phenylbutazone,b flunixin meglumine,c dimethylsulfoxide (DMSO),d and acepromazine.e4 Unfortunately, there are no pharmacological agents that are of proven benefit after the initiating events have occurred. The purported anti-inflammatory, diuretic, and oxygen radial scavenging properties of DMSO make it a logical choice. Experimentally, acepromazine increases digital and laminar blood flow in normal horses, but it has not been tested in horses with induced laminitis.9 Horses that have developed laminitis associated with insulin resistance, such as in equine metabolic disease, may benefit from early intervention to increase insulin sensitivity.7 Measures should be taken immediately to reduce the weight of obese horses. The use of ice therapy in the acute stage of laminitis has been described, but its use outside of the developmental stage remains somewhat controversial.7
Radiographs
Baseline radiographs consisting of a lateral and dorsopalmar(DP) 0° view should always be taken during the initial examination of acute laminitis if possible.3 The radiographs can be used to determine previous damage, assess foot conformation, and guide initial hoof care. Serial radiographs taken at 2- to 4-day intervals during the instable period are used to follow the progression of displacement and speed of progression of the distal phalanx. Venography can be used to assess the circulatory pattern of the foot, but the clinician must be experienced in performing the procedure and interpreting the results.
 |
| Fig. 2. Creased nail puller with short handles. |
 |
| Fig. 3. Schematic representation of a laminitic horse standing in sand. Note that the properties of sand contour to the solar surface of the foot and allow the horse's toe to sink in the sand and elevate the heel. (Courtesy of Andrew Parks.) |
 |
| Fig. 4. Wooden shoe attached to the foot with screws placed around the perimeter of the hoof wall and secured with casting tape. |
Hoof Care
Physical measures are often applied to the foot by the attending or consulting veterinarian during the acute stage of laminitis. The greatest overall stresses placed on the foot are associated with weight-bearing. To limit the focally increased stresses placed on the foot during ambulation, it is imperative that an acute laminitic horse be restricted to the stall. When a horse is shod or standing on a hard surface, the load is concentrated around the perimeter of the hoof wall and transferred onto the lamellae. In acute laminitis, it is appropriate to remove the shoes, which is readily accomplished by removing individual nails with a short-handled crease nail pullerf (Fig. 2). If the horse is in extreme pain and reluctant to lift a foot, local anesthesia should be avoided, and sedation, such as detomidine hydrochloride,g should be used to allow for removal of the shoes. Weight can be redistributed to the palmar/plantar section of the foot by applying some type of deformable material to the solar surface of the foot such that the sole, bars,and frog in the palmar section of the foot become load-sharing with the hoof wall. This redistribution can be accomplished by applying thick Styrofoam, deformable impression material, or various pads and boots that are marketed for this purpose or placing the horse in sand (Fig. 3). The author prefers to use beach sand if available. Caution must be used when employing the dorsal area of the sole distal to the dorsal margin of the distal phalanx and the adjacent wall to bear weight. It should be noted that recent biomechanical research has shown that, when the foot is loaded, the hoof expands or flares out, and as a result, it pulls the sole distally.10 Therefore, applying pressure to the sole in a horse with minimal sole depth or one that shows pain when hoof testers are applied may, in fact, compromise circulation and increase the pain level. Applying shoes in the acute stage of laminitis has not been shown to offer any advantages. In the acute stage of laminitis, the moments about the DIP joint and the distractive force placed on the lamellae by the DDFT can be reduced to some extent by moving the breakover in a palmar/plantar direction. A line is drawn across the solar surface of the foot dorsal to the frog, and a rasp is used to bevel the toe in a dorsal direction from this line until it is approximately 25-30° to the ground. This bevel effectively moves the breakover palmarly, decreases the pressure on the dorsal lamellae, and may lessen the forces created by the DDFT. Additionally, beveling the toe in this manner reduces weight-bearing by the dorsal wall at rest. The center of pressure is effectively moved in a palmar direction by extending the ground surface of the foot palmarly and applying mild heel elevation. Raising the heels excessively in the acute stage has been advocated but should be done with caution, because there is no scientific proof of a beneficial effect.
Laminitis as a consequence of various systemic diseases and/or the administration of corticosteroids often results in distal displacement (sinking) of the distal phalanx. In this case, the entire circumferential lamina interface is damaged, allowing the distal phalanx to descend or sink uniformly within the hoof capsule. There is minimal involvement of the DDFT during this process. The author has not found elevating the heels in horses with distal displacement to be effective. Moving the breakover back and placing a uniform layer of a deformable impression material on the bottom of the foot or placing the horse in sand may be a better option.4
Recently, the author favored the use of a wooden block or shoe in horses with acute laminitis that are expected to rotate or sink, and the results have been very encouraging. The flat solid construction allows the entire ground surface of the foot to be used for weight-bearing without excessive pressure on the sole. The border of the ground surface of the wooden shoe can be beveled or cut on an angle, which seems to concentrate the load under the digit. The wooden shoe can be applied in a non-traumatic manner, and the angle around the periphery of the shoe seems to decrease torque on the lamellae in the toe and quarters. Two-inch fiberglass casting tape is used to secure the block and limit expansion of the foot (Fig. 4).
An acute case of laminitis should be reevaluated at 48-72 h for improvement or worsening of the condition. If the horse has not shown marked progress, the horse should be reassessed by the responsible parties regarding treatment plans and alternatives. The prognosis becomes less optimistic.The client should also be aware that referral facilities exist that provide additional options.
7. Chronic Laminitis
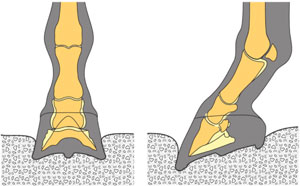
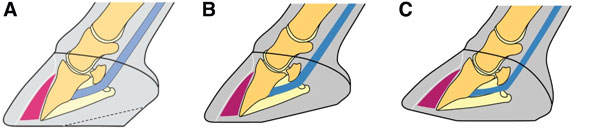
Rehabilitation of the horse with chronic laminitis is not a cookbook process, because affected horses with chronic laminitis will vary from case to case and our understanding of the disease is still vague. However, the understanding of digital mechanics has improved, and technological advances in shoe design/materials and techniques continue to expand. Chronic laminitis by definition means that the distal phalanx has displaced within the hoof capsule.11 The distal phalanx can rotate down at the toe, rotate to either side (laterally or medially), or totally displace (sink) within the hoof capsule (Fig. 5). Rehabilitation of the horse with chronic laminitis will depend on the amount of viable lamellae that remain intact, the conformation of the foot, and the ability to realign the distal phalanx within the hoof capsule. The question is often asked as to when to shoe a horse with chronic laminitis. The guidelines that may be used are when the horse is comfortable (stability), the horse is on minimal medication, and the foot has been stabilized (i.e., there have been no additional radiographic changes in the foot for a given period of time). The author has not been successful or observed improvement in the laminitic state of any horse when having to use local anesthesia to lift the horse's foot and apply a shoe before the foot has stabilized.
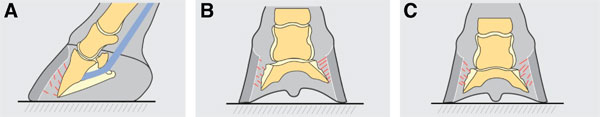 |
| Fig. 5. (A) Dorsal capsular rotation, (B) mediolateral rotation, and (C) distal displacement are illustrated. |
 |
| Fig. 6. Radiograph of asymmetrical displacement of the distal phalanx on the medial side. Note that the solar foramens are not parallel with the ground. Also note the disparity in the joint space from the lateral to the medial side. |
 |
| Fig. 7. A schematic representation of a lateral radiograph of a foot with dorsal capsular rotation can be used as a template when trimming. A line is drawn approximately parallel and about 15 mm distal to the solar surface of the distal phalanx. A second line is drawn parallel and approximately 15-18 mm dorsal to the parietal surface of the distal phalanx. The arrow at the intersection of the two lines is the farthest dorsal point that the toe of the shoe should be set. The second arrow is approximately 6 mm dorsal to the dorsal margin of the distal phalanx, and it is the approximate location of the point of breakover. (Courtesy of Andrew Parks.) |
Radiology
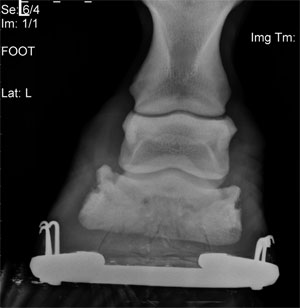
The lateral radiograph is often the only film taken for evaluating chronic laminitis, but it does not allow identification of asymmetrical medial or lateral distal displacement. Therefore, the author considers it crucial that a DP radiographic projection is included as part of the radiographic study for either acute or chronic laminitis.12 High-quality radiographs are required to visualize the osseous structures within the hoof capsule as well as the hoof capsule itself. The radiographic features of chronic laminitis are well-documented.13 The following observations from the lateral radiograph are important in determining the prognosis and guiding treatment: the thickness of the dorsal hoof wall,the degree of dorsal capsular rotation, the angle of the solar surface of the distal phalanx relative to the ground, the distance between the dorsal margin of the distal phalanx and the ground, and the thickness of the sole.
The DP radiograph is examined to determine the position of the distal phalanx in the frontal plane. Asymmetrical distal displacement of the distal phalanx on either the lateral or medial side is present if a line drawn across the articular surface of the DIP joint or between the solar foramens of the distal phalanx is not parallel to the ground, the joint space is widened on the affected side and narrowed on the opposite side, and the width of the hoof wall appears thicker than normal on the affected side (Fig. 6).
Finally, radiology will form the guidelines to be used in realigning the distal phalanx and applying any type of farriery (Fig. 7).
Farriery for Chronic Laminitis
Trimming and shoeing has always been the mainstay of treating chronic laminitis, and it is directed at reducing/removing the adverse forces on the compromised lamellae. In considering hoof care in horses with chronic laminitis, there are three goals for therapy: to stabilize the distal phalanx within the hoof capsule, control pain, and encourage new hoof growth to assume the most normal relationship to the distal phalanx possible.12 Realignment of the distal phalanx to create a better relationship of the solar surface of the distal phalanx with the ground is used as the basis for treating chronic laminitis.14,15 Realignment of the distal phalanx should promote and produce hoof wall growth at the coronet and sole growth distal to the distal phalanx. Using the radiographs as a template, the objective of the trim is to reposition the distal phalanx within the hoof capsule and realign the ground surface of the hoof capsule with the solar margin of the distal phalanx (Fig. 8). Applying any type of shoe after this procedure should complement the realignment of the distal phalanx and decrease the forces on the lamellae. The shoeing principles applied to all shoeing methods used in treating chronic laminitis are to recruit ground surface, reposition the breakover palmarly, and provide heel elevation as needed.12,14 The author's shoe of choice is usually a wide-web aluminum shoe with heel elevation either incorporated into the shoe in the form of rails or by using a bar wedge inserted between the shoe and the solar surface of the foot. Deformable impression materialh can be applied between the branches of the shoe to increase the surface area and redistribute the load. Breakover can easily be placed into the shoe in the appropriate place by forging or using an electrical grinder. The middle of the foot is used for accurate placement of the shoe on the foot.12
Recently, the author has been very successful at treating selected cases of chronic laminitis using a wooden block cut in the shape of the foot with the border of the ground surface cut on an angle of at least 45° (Fig. 9).12,14,16,17 The foot is trimmed appropriately to address realignment; impression material is used judiciously in the palmar section of the foot to create a solid plane between the solar surface of the foot and the wooden shoe. Heel elevation can be incorporated into the wooden shoe if necessary, and the shoe is applied a traumatically using screws and casting tape. With this method, there is flat, even pressure placed across the palmar section of the foot, and all the mechanics are placed in the block while preserving the hoof capsule.
 |
| Fig. 8. A schematic diagram of a horse's foot with rotation before (A) and after being trimmed (B) according to guidelines in Fig. 7. Note that in C, the dorsal and palmar aspects of the ground surface now form two different planes. (Courtesy of Andrew Parks.) |
 |
| Figure 9. A wooden shoe applied to the foot. Note the screws are inserted against the hoof wall and the point of breakover on the ground surface of the shoe corresponds with a vertical line drawn from the coronet. |
 |
| Fig. 10. Lateral and DP radiograph of a horse with severe laminitis. The displacement of the distal phalanx, the position of the coronet, the disruption of the lamellae, and the solar penetration will prevent recovery. |
Surgery
DDF tenotomy remains a very useful procedure for treating chronic laminitis. The author considers this surgery necessary if the margin of the distal phalanx has prolapsed through the sole or in those cases that fail to stabilize after they begin displacing. As stated earlier, two of the main detriments when treating chronic laminitis are the weight of the horse and the distractive force of the DDFT. One of these detrimental forces can be removed through this surgery, but knowing when to use it poses a dilemma. It is often necessary to use this procedure to realign the distal phalanx. Additional indications for this surgery are progressive rotation, persistent pain, minimal hoof wall and/or sole growth, and secondary flexor apparatus contracture. If there is a marked flexural deformity involving the DIP joint present, it indicates shortening of the musculotendonous unit, and a release procedure is necessary to accomplish realignment of the distal phalanx. It has to be emphasized that, if a DDF tenotomy is used, it must be accompanied by realignment of the distal phalanx to decrease the adverse forces on the lamellae. After a DDF tenotomy, the middle phalanx will move distally and palmarly relative to the distal phalanx. This movement concentrates the load on the palmar soft-tissue structures of the foot rather than redistributing the load on the solar surface of the distal phalanx. The author has found it helpful to use a shoe or wedge pad attached to a cuff to extend the ground surface beyond the heel of the hoof capsule and add a few degrees of heel elevation. This elevation will realign the digital axis, and it seems to improve the clinical parameters (comfort, hoof capsule changes, sole growth, etc.) after surgery.12
Ethical Considerations
The clinicians should continually discuss the humane issues surrounding a case of severe laminitis from the onset. This discussion is especially important in laminitis cases that have the potential or are displaying clinical and radiographic signs of distal displacement (sinking), because these cases inevitably have a poor prognosis. From a humane aspect, it is irresponsible to prolong the life of a chronically painful horse with no chance of recovery or any quality of life. The decision for euthanasia is often subjective, and the clinician must take into consideration the owner's psychological attachment to the horse. Monetary and insurance considerations must be discussed frankly. Convincing evidence can and should be presented to the owner, such as duration of the current treatment, status of the horse (unrelenting pain, recumbency, or weight loss), foot conformation (no hoof or sole growth, prolapse of distal phalanx through the sole, or palpable trough at the coronet), and imaging (severe displacement-rotation and/or sinking, position of coronet,or irreversible damage to the hoof capsule) (Fig. 10). If a decision is reached to euthanize a horse, the decision should be unanimous among all the members of the team. The clinician should recommend and encourage the owner to seek a second opinion.The attending or consulting veterinarian or farrier should never imply to the owner that a different approach or mode of therapy initiated at a particular time would have changed the outcome of the case. There is no scientific evidence to support such a derogatory statement, it casts doubt on the professionalism of the clinicians involved, and it opens the door for possible litigation.
8. Discussion
Unfortunately, many of the treatment regimens, both medical and farriery techniques, used to treat acute and chronic laminitis are based on tradition, theoretical assumptions that a given treatment should work, and anecdotal evidence that a certain type of treatment has worked on previous cases.There are no controlled studies confirming or comparing the efficacy of the numerous treatments in use, and there is no scientific proof that one treatment is superior to another treatment. What is well-documented are the forces and mechanics applicable to the equine foot. Clinicians (veterinarians and farriers) may be better served by a thorough knowledge and understanding of the anatomy, physiology,and function of the hoof. Understanding the foot in a mechanical sense may allow for better application of a preferential treatment protocol.
Treatment of laminitis has to be a team effort equally shared between veterinarian, farrier, and owner. The intent of this paper is not to discourage treatment of laminitis but to create expectations that are realistic, humane, and based on the cause of the disease, amount of lamellar damage, pain, duration, and financial constraints involved in prolonged treatment. At the onset of treating severe laminitis, certain guidelines can and should be outlined to indicate the efficacy of the chosen treatment method along with a reasonable time frame for improvement. These guidelines could be a change in stance, decreased digital pulse, increased comfort, horn growth at the coronet, sole growth, etc. If the desired improvement is not observed or the condition gets worse, the overall farriery methods should be reassessed and changed where necessary.
With severe laminitis cases, we are often unable to rehabilitate the horse to where it has an acceptable quality of life. The main reason is that there are insufficient laminar structures remaining within the hoof to achieve realignment and accept weight. The author feels that it is important, from a humane perspective, to know when to discontinue treatment that has not been effective. Often, we persevere with various treatments, putting the horse through much unnecessary suffering, only to achieve an unsatisfactory outcome. It is unlikely that this disease can ever be fully eliminated, and it is unlikely that there will ever be a single drug or other line of therapy to consistently treat acute or chronic laminitis; therefore, our clinical and research efforts should be divided between prevention and treatment.
References and Footnotes