Andrew H. Parks, MA, Vet MB
1. Introduction
Most equine clinicians are familiar with the healing and treatment of traumatic wounds to the distal limb, proximal to the foot, because the general principles of wound healing are well taught in veterinary schools. This receives constant reinforcement as these wounds are a weekly if not daily occurrence in general practice. Foot wounds, though less frequently encountered, are not uncommon. Unfortunately, they are often treated hesitantly by practitioners, presumably because of misunderstanding or unfamiliarity, so that the treatment is ineffective. This is probably because little time is spent relating the principles of healing to the treatment of foot wounds in already overcrowded college curricula, because the morphologic differences between the integument of the foot and skin is confusing, and because experience with management of such wounds in practice is less common.
It is unfortunate that the gross morphologic differences between the integument of the foot and the skin belie the overwhelming similarities, both in structure and response to injury. To overcome any misunderstanding based on the morphological differences, the author finds it simplest to relate the less familiar foot wounds to the well understood more proximal limb wounds, to emphasize the similarities and then point out the differences. To this end, it is pertinent to review the anatomy and general classification of wounds before discussing wound healing and treatment. Unfortunately, there is little or no information from research on the way foot wounds heal, so that practical treatment of foot wounds must be based on experience and extrapolation from research on skin wounds.
2. Anatomy of the Integument
A. Skin
The skin is composed of three layers, epithelium, dermis and tela subcutanea (subcutaneous tissue). The epithelium is subdivided into 5 layers: stratum basale, stratum spinosum, stratum granulosum, stratum lucidum and stratum corneum that reflect the progression from the germinal cells at the base to the fully differentiated cornified cells superficially. The epithelial layer is sharply demarcated from the dermis between which is interposed the basement membrane. Dermal projections of various lengths and widths, called papillae, extend superficially into the epidermis. The epidermis that interdigitates with the dermal papillae forms the epidermal pegs. The deeper layers of the dermis blend with the subcutaneous tissue, which in turn is loosely attached to the underlying fascia. Epithelial elements, namely glands and hair follicles, extend into the dermis and subcutaneous tissue. The general architectural pattern of the skin described here is similar across most of the body surface though the relative thickness of the layers and density of the adnexal structures varies. The stratum corneum of the skin is continually replaced by multiplication and differentiation of cells from the deeper layers of the immediately underlying epidermis to replace the stratum corneum as it exfoliates superficially.
B. Integument of the foot1,2
Like the skin, the integument of the foot is also composed of 3 layers: the epidermis, dermis and subcutaneous tissue. Similarly the epithelium is subdivided into layers, though over most of the surface of the foot, only three layers are recognized: the stratum basale, stratum spinosum and stratum corneum. The stratum basale and stratum spinosum are frequently referred to together as the stratum germinativum. It is the stratum corneum of the foot that forms the hoof capsule.
Within this common framework of the integument, the structure of the integument of the foot is highly specialized both because of its difference as a whole to the skin and because of the differences between the regions within the foot. Unlike the relative topographical uniformity of skin, the structure of the integument of the foot is divided topographically into several regions: periople, coronary band, wall, sole, frog and heel bulbs. These divisions reflect the differences in appearance, structure and function of the different portions of the integument of the foot rather than the nature of the underlying germinal epithelium and dermis. The integument of the foot is divided into 5 types, perioplic, coronary, laminar, solar and cuneate that are continuous with one another but the boundaries are abrupt.
Just as the dermal papillae of the skin interdigitate with the epidermal pegs, so the dermis and epidermis of the integument of the foot interdigitate. However, the interdigitation between the dermis and epidermis of the integument of the foot is more regular and highly specialized. The perioplic, coronary, solar and cuneate dermis all form long thin filament-like papillae that project distally into corresponding pockets in the epidermis. The germinal epithelium on the sides of the dermal papillae forms the horn tubules. The germinal epithelium that abuts the dermis between the base of the dermal papillae forms the epidermal pegs that generate the intertubular horn. The laminar dermis is folded into longitudinal ridges, called the primary dermal laminae, that extend from the junction of the laminar dermis with the coronary dermis proximally to its junction with the solar dermis distally. The surface of each dermal laminae is further folded into many secondary ridges, called secondary laminae, on both sides and on the tips of the primary dermal laminae. The infolding of the epidermis that follows the contour of the dermis forms the primary and secondary epidermal laminae. Only the primary epidermal laminae are keratinized.
The subcutaneous tissue of the integument of the foot is also highly specialized and forms the modified periosteum of the distal phalanx and the perichondrium of the collateral cartilage. The cuneate subcutaneous tissue forms the digital cushion.
The stratum corneum of the integument of the foot is replaced by the germinal layer as it is in the skin. However, while the relationship between new stratum corneum formation and the immediately underlying epidermis is obvious for the sole and frog, this relationship is not immediately perceived as being as straightforward for the wall because the wall is derived from epithelium of three types: the outer layer, the stratum externum, is the stratum corneum of the perioplic epithelium; the middle layer, the stratum medium, is the stratum corneum of the coronary epithelium; and the inner layer, the stratum internum, is the stratum corneum of the laminar epithelium. However, the plane of the perioplic and coronary epithelium is almost perpendicular to the plane of the laminar epithelium so that all 3 cannot proliferate and increase in thickness perpendicular in the same manner as skin. The stratum externum and stratum medium are replaced in a similar manner to skin, i.e. the direction of growth or replacement is perpendicular to the plane of the epithelial layer. In contrast, the laminar epithelium undergoes limited proliferation which is concentrated near its junction with the coronary epithelium.
3. Classification of Wounds
Open wounds have been classified in various ways including etiological appearance, depth and degree of contamination. For the purpose of comparing skin wounds to foot wounds with a later view to comparison of the mechanisms of wound healing is beneficial to discuss both the depth and etiological appearance of wounds in the skin, followed by comparison with the foot.
A. Wounds involving the skin
Wounds that cause defects characterized by tissue loss may be classified as partial or full thickness wounds. Partial thickness wounds of the skin involve loss of the epidermis and partial loss of the dermis, but truncated adnexal epidermal elements are still present in the dermis. Full thickness wounds extend through the epidermis and dermis to the subcutaneous tissue and may involve any other underlying structures.
By etiology, wounds are subdivided into abrasions, incisions, lacerations, avulsions and punctures. Abrasions involve loss of the epidermis and portions of the dermis. The deeper portions of epidermal adnexal structures persist across the surface of wound in the dermis and in the subcutaneous tissues. Incised wounds in the skin, typified by a scalpel incision, have smooth margins that gape, sever all soft tissues in the wound, and extend to varying depths.
Lacerations are caused by the tearing of the skin and underlying soft tissues so that they have irregular margins and are often accompanied by surrounding soft tissue trauma. Avulsions are similar to lacerations except that more superficial tissues are torn from their attachments to the deeper structures and the blood supply is more likely to be compromised than a straightforward laceration.
Puncture wounds are characterized by a small entry wound that gives no indication to the depth or direction of the underlying trauma and are highly likely to be contaminated.
B. Wound involving the foot
The thickness and the biomechanical properties of the stratum corneum of the foot affect the pattern of injury seen in the equine foot. The thick stratum corneum deflects many minor blows that might injure the skin, and any small defects that occur in the outer layers of the stratum corneum are of no clinical significance. The biomechanical properties of the tubular and intertubular horn of the wall are such that cracks in the stratum corneum caused by more serious injury are deflected outwards to the exterior surface of the foot away from the sensitive dermis. It is also the structural nature of the stratum corneum of the foot wall that causes it to fracture along predetermined planes rather than tear irregularly.
Stump asserts that when the horny layer of the epidermis is separated from the foot, either by maceration, accident or surgery, the separation occurs between the stratum corneum and stratum germinativum;2 a clinical example would be the defect caused by hoof wall ablation with a cast cutter. This would not classify as a partial thickness wound because the germinal layers of the epithelium would not be breached. In fact, because the integument of the foot does not have adnexal epidermal structures that project into the dermis and subcutaneous tissue except for the merocrine glands present in the frog, a direct corollary of the classical partial thickness skin wound does not exist in the foot. However, in an injury that removes most of the epidermis, but leaves islands of the stratum germinativum of the epidermal pegs or secondary laminae attached to the dermis might be expected to heal in a similar manner to partial thickness skin wounds. In contrast to Stump's assertion, it is the author's experience that most surgically created defects, except for the drainage of foot abscesses, and many naturally occurring foot wounds are full thickness injuries.
Abrasions to the coronary band are the most likely injury to resemble partial thickness wounds occur because the integument is thinnest at the coronary band. Where the integument is thicker, in the author's experience, any injury of sufficient force to damage the full thickness of the wall frequently creates a full thickness wound.
Incised wounds to the integument of the foot are very uncommon, but when they occur the rigidity of the stratum corneum of the foot prevents the margins from gaping. An example of such a wound would occur if a horse kicked against an edge of sheet metal.
Lacerations of the integument of the foot are less common than they are in skin because the rigid nature of the stratum corneum causes the hoof to fracture rather than tear, which usually causes the tissues to avulse from the underlying structures. Lacerations to the pastern, however, are quite common, most commonly involve the heels, and may extend distally through the coronary band.
Avulsions of the hoof wall are not uncommon and usually involve the wall at the quarters or heels. They may extend proximally to involve the coronary band and / or distally to involve the sole. Avulsions may be complete or incomplete. In complete avulsions, the affected wall and attached structures are completely separated from the foot. Incomplete hoof wall avulsions remain attached to the foot along at least one or more margin, usually proximally.
Puncture wounds are common injuries to the ground surface of the foot and occasionally occur at the coronary band, but are rare in the wall. They may only be apparent as a small dark spot on the horn of the sole, and if they occur in the frog, the softer horn may close over the original injury.
4. Wound Healing
A. General principles as applied to skin wounds
The healing of full thickness wounds is classically divided into 4 phases: Inflammation, debridement, repair and maturation.5 In the inflammatory phase an initial vasocontriction to minimize hemorrhage is followed by vasodilation and white cells migrate and plasma proteins leak into the wound. The protein together with the red and white cells from the wound forms a clot which later contracts to form a scab that protects the surface of the wound. In the debridement phase bacteria, blood clots, and necrotic and foreign material are removed from the wound through phagocytosis by white cells, sloughing or surgical debridement.
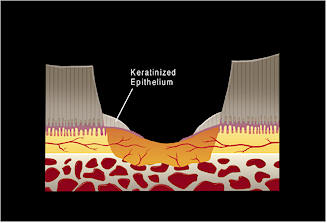
The repair phase is itself a combination of three processes, contraction, fibroplasia and epithelialization. Wound contraction occurs through the action of myofibroblasts which actively develop tension in the periphery of the wound that causes centripetal movement of the wound margins over the granulation tissue surface. Fibroplasia occurs at the surface of almost all healthy debrided wound surfaces deep to the epithelium. Fibroblasts, differentiated from mesenchymal cells, proliferate at the surface of the wound and migrate along the fibrin lattice in the wound. This is rapidly followed by the development of new capillaries by endothelial budding. Together the fibroblasts and capillaries form granulation tissue. Although granulation tissue forms on the surface of almost any healthy tissue in the wound, it proceeds more rapidly from highly vascular tissues such as the subcutaneous tissue and more slowly from less vascular tissues such as tendon or bone. Collagen secretion by the fibroblasts during this phase of wound healing causes the rapid gain in wound strength. Epithelialization occurs by proliferation of epithelial cells at the periphery of the wound which then migrate across the surface of the granulation tissue. As the margin of the newly formed epithelial surface encroaches on the center of the wound, the epithelial cells towards the periphery of the wound proliferate so that the epithelium increases in thickness.
In the maturation phase the vascularity and cellularity of the wound decreases as wound continues to gain in strength, though at a slower pace, as the collagen reorganizes and forms crosslinks.
The healing of partial thickness skin wounds follows a somewhat different pattern to full thickness wounds.6 Because full thickness of the dermis has not been lost and severed epithelial adnexal structures persist in the dermis, the epithelium proliferation occurs at the margin of the wound and at the margins of the truncated epithelial structures. Because dermal tissue persists across the surface of the wound, the proliferating epithelium is able to migrate across the surface of the dermis without granulation tissue forming in the wound and it is not until the wound is completely epithelialized that a fibroblastic reaction occurs in the dermis. Wound contracture is limited compared to full thickness wounds.
B. General principles as applied to foot wounds
Foot wounds follow the same four basic processes. The differences that are apparent primarily relate to the rigid nature of the stratum corneum and the variety of epithelial types found in the foot and the pattern of replacement of the stratum corneum . In the inflammatory phase, wounds below the coronary band are contained within the rigid stratum corneum of the foot so the tissues within the hoof are unable to swell. In the debridement phase, the rigid nature of the hoof may impede drainage of exudate and the sloughing of necrotic or foreign material from wounds.
In the repair phase, contraction does not occur.7 The most apparent difference between healing of skin and foot involves epithelialization. Epithelium migrates across the surface of a wound in the foot just as it does in the skin. However, the epithelial margin of a skin wound is usually relatively homogenous whereas the epithelium at the margins of a foot wound may be of one or more types. The simplest example would be a defect confined to a single epithelial type, either the sole or frog. The epithelial margins wound then be of a uniform type so that epithelial coverage of the wound would be very similar to a full thickness skin wound except for the greater thickness of stratum corneum to be replaced.
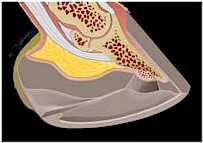 (a)
| Figure 1. A schematic representation of a full thickness wound to the sole that extends to the distal phalanx. a) Orientation to the location of the wound. b) The initial defect devoid of clot and exudate. c) Initial fibroplasia and epithelialization from the wound margins. d) Fibroplasia from both the margins of the wound and the distal phalanx fill the defect. The epithelium has migrated further across fibroplastic tissue in the defect; at the periphery of the wound, the epithelium has increased in thickness and the superficial layers keratinized. e) Epithelial migration is complete. f) Full thickness of the epithelial defect is re-established by epithelial proliferation. 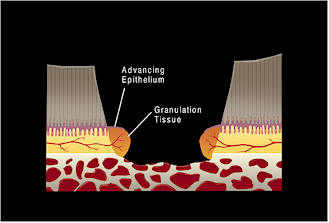 (c)
 (d) |
A full thickness wound to the wall that does not involve either the sole or the coronary band forms a defect in all three layers of the wall but only involves the germinal layer of the laminar epithelium . Therefore, the defect will be epithelialized by laminar epithelium. However, because the laminar epithelium is only capable of limited proliferation, the defect in the stratum internum is closed, but the defects in the stratum externum and stratum medium persist moving distally with normal hoof wall growth until the wall proximal to the defect has reached the weight-bearing surface of the hoof.
| Figure 2. a) A schematic representation of a wound that extends deep to the epidermis and dermis of the wall into the modified subcutaneous tissue. b) Fibroplasia occurs simultaneously from the margins and depth of the wound. Epithelial cells from the adjacent laminar epithelium at the margin of the injury migrate over the fibroplastic tissue to replace the stratum internum. Concurrently, the stratum medium, derived from the coronary epithelium, continues to migrate distally in the normal pattern of hoof wall growth. c) Once the laminar epithelium has fully replaced the stratum internum, the defect in stratum medium migrates distally until it is completey replaced when the stratum medium that was originally proximal to the injury reaches the solar margin of the hoof.
|  (a)
 (b)
 (b) |
If the margins of a wound are composed of more that one source of epithelium, it appears that the nature of the newly formed stratum corneum reflects the source of epithelium that migrated to fill the defect. Nowhere is this more apparent than wounds that involve the skin of the pastern and the coronary band ; it is not uncommon for epithelium to migrate proximally to the previous margin of the coronary band to for a spur of horn in the distal pastern. Likewise if a defect in the coronary band is not filled with coronary epithelium, a persistent defect in the hoof wall may develop.
5. Treatment of Wounds
A. General treatment of skin wounds
Many factors, both local and systemic, influence the way wounds heal.5 The systemic influences on wound healing are beyond the scope of this discussion. It is the clinician's task to manipulate the local factors affecting wound healing to achieve the fastest wound closure compatible with the best possible functional outcome. To this end, wound debridement, closure, bandaging, and medical treatment must all be considered.
| Figure 3. a) A schematic representation of a complete hoof wall avulsion at the heel. The injury involves the integument of the pastern, coronary band, wall and sole. b) Fibroplasia proceeds as previously described and epithelialization occurs from the periphery of the wound. c) The final appearance and structure of the healed injury appears to reflect the nature of the epithelium that migrated to close each part of the defect.
|  (a)
 (b)  (b) |
The objective of wound debridement is to remove as much necrotic tissue, foreign material, and infection as possible. This is usually accomplished by wound lavage and surgical excision. If tissue viability is questionable and it can be excised without endangering other nearby structures it should be removed, but if tissue of questionable viability is adjacent to a vital structure, such as a joint capsule, it is better left and observed and may be debrided at a later date.
If wound contamination and tissue injury do not preclude it, wound closure almost always provides the most rapid and functional result. The wound closure may be primary or delayed primary.
Bandaging serves many functions including wound protection from trauma and desiccation, applying pressure to the wound surface, wicking away exudate, and maintaining dressings and topical medication in place. Typically, distal limb bandages are composed of 3 layers, a surface dressing, a layer of sheet or roll cotton to distribute pressure and absorb moisture, and an elastic layer to maintain the bandage in place and apply pressure. Surface dressings influence, debridement, contraction, fibroplasia and epithelialization of wounds healing by secondary intention. Adherent dressings are frequently used to lift necrotic debris off from a wound surface. Once a wound is debrided, contraction proceeds faster under a petrolatum impregnated gauze, but once wound contraction is complete epithelialization proceeds more rapidly under a Telfa pad.
Topical antibiotics and antiseptics are available as solutions, ointments and creams. Ointments and creams are easier to apply and maintain on a wound surface, but gentamicin solution has been proven to be superior to a gentamicin cream. The author favors solutions because they dilute exudate and help to maintain a physiological environment at the wound surface. Topical antiseptics are very effective in low concentrations, for example, 0.1 - 1% povidone iodine or 0.05% chlorhexidine but are deleterious at higher concentrations. In general, astringents and caustics are deleterious to fibroplasia and epithelialization and their use should be avoided. Systemic antibiotics are seldom warranted in the treatment of wounds that are confined to the integument.
B. Treatment of foot wounds
Foot wounds warrant special consideration because the foot is in constant contact with the ground and because of the structure of the stratum corneum of the integument of the foot. In addition, there are several traditional practices that are applied to foot wounds that most practitioners would not consider doing to other wounds. The debridement of foot wounds closely follows the general principles, but caution must be taken when debriding deeper wounds because of the close proximity of many vital structures. The practice of soaking horse's feet in buckets of water with or without antiseptics to lavage a wound is questionable under any circumstance, but soaking feet with wounds to deeper structures such as the navicular bursa cannot be recommended.
Wound closure is seldom possible or necessary so that most are left to heal by secondary intention. The exception is injuries to the coronary band which should be reconstructed wherever possible to retain the greatest functional capabilities of the digit. The coronary band can be readily sutured proximally where it is thin, but the hoof wall may need to be shaved more distally to allow the placement of sutures. The closure may be primary or delayed primary. Any avulsed wall distal to the coronary band will not reattach to the foot so it may be removed unless it is required to maintain the normal orientation of the coronary band.
Bandaging horse's feet follows similar principles to the rest of the distal limb except that the middle layer is frequently omitted. Any topical medication that serves to treat other distal limb wounds may be applied with similar considerations. The use of full strength povidone iodine or topical astringents is usually deleterious and should only be used with considerable caution, especially when the integument has been breached. The author's preference is a dry to dry, or wet to dry dressing with a Telfa pad. Wet to dry dressings are readily applied by first applying the Telfa pad, cotton gauze backing and roll gauze dry before moistening the dressing, which is then achieved either by pouring or spraying the solution on top of the dressing. Because moisture from stall bedding readily seeps into any foot bandage, the application of piece of rubber inner tube or treatment plate is advantageous; taping on the first wedge and cuff of a Redden Modified Ultimate works very well. Once a wound has completely epithelialized, topical astringents such as 2% iodine may be applied with caution to toughen up the newly formed stratum corneum. Bandages do not always provide satisfactory stability to the foot capsule for wounds involving the coronary band so that casting with a digital cast is employed to decrease the likelihood of persistent hoof wall defects.7,8
The use of antibiotics at all in foot wounds has been questioned.9 However, most clinicians would recommend systemic antibiotics if the wound breaches the integument until the entire surface of the wound is covered by granulation tissue, and most would consider systemic antibiotics imperative if a joint, tendon sheath or bursa is involved.
6. Complications
A. Distal limb wounds proximal to the foot.
The most likely complications to occur are a delay or cessation of closure in wounds healing by secondary intention, breakdown of sutured wounds, and a loss of function due to fibrosis in the wound. Wounds left to heal by secondary intention on the distal limb of horses heal notoriously slowly. This is in part due to innate features of wound healing in the distal limb of the horse. Wound contraction in the distal limb is limited compared to wounds of the trunk because of the tension in the skin. Also, exuberant granulation tissue is common and it prevents wounds from epithelializing satisfactorily. In addition, the presence of infection, necrotic debris or foreign material will impede wound healing. Inadequate protection of the wound will desiccate the wound surface and may allow further wound trauma to occur.
B. Foot wounds
Most of the complications seen in the healing of foot wounds are the same that occur in skin wounds. Many full thickness foot wounds also heal slowly. While wound contraction is absent in foot wounds, exuberant granulation tissue is seldom a problem. Being in constant contact with the ground the foot is inherently predisposed to further injury. Occasionally wound closure appears to be arrested for no apparent reason; these wounds usually respond to light surface debridement and bandaging with a wet to dry dressing.
After the wound has completely healed, the foot may not function normally if the hoof is unable to evenly support the distal phalanx or if injury to the deeper structures has interfered with attachment of a structurally sound hoof to the distal phalanx. Therapeutic trimming and shoeing with bars, clips or extensions may be needed to minimize any functional deficits.
7. Conclusion
By combining knowledge about the anatomy and function of a horse's foot with knowledge about the principles of healing in skin wounds, sound decisions can be made about the treatment of foot wounds when specific information is not available that result in satisfactory clinical outcomes.
References
1. Habermehl, K-H. The digital organ of the horse. In: The anatomy of Domestic Animals, Volume 3, The Circulatory system, the Skin, and the Cutaneous Organs of Domestic Animals. Ed. R. Nickel, A. Schummer and E, Seiferle. New York, Springer - Verlag, 1981: 541-550.
2. Stump JE. Anatomy of the normal equine foot, including microscopic features of the laminar region. J. Am. Vet. Med. Assoc. 1967; 151: 1588-1598.
3. Pollitt CC. The anatomy and physiology of the hoof wall. Equine Vet Education Manual No 4. 1998; 3-10.
4. Waldron DR, Trevor T. Management of superficial skin wounds. In: Textbook of Small Animal Surgery. Ed: D. Slatter. 2nd edition. Philadelphia, W.B. Saunders Company, 1993; 269.
5. Stasha TS. Equine Wound Management. Philadelphia, Lea and Febiger, 1991: 1-18, 19-34.
6. Gilman T. (1968) Partial thickness loss excised wounds. In: Healing of Cutaneous Wounds. Greenford, Glaxo Laboratories, 1968; 16-20.
7. Fessler JF. Hoof injuries. Vet Clin N. Am.: Equine Pract. 1989; 5: 643-664.
8. Steckel RR, Fessler JF. Surgical management of severe hoof wounds in the horse: a retrospective of 30 cases. Comp. Cont. Educ. Pract. Vet 1983; 5: S435-S443.
9. Blackford JT, Latimer FG, Wan PY, Shires GMH. Treating pastern and foot lacerations with a phalangeal cast. in Proceedings 40yh Annu Conv Am. Assoc Equine Practnr. 1994; 97-98.