Hoof Abscesses:A Practical ApproachReprinted with permission from the American Farriers Journal. |
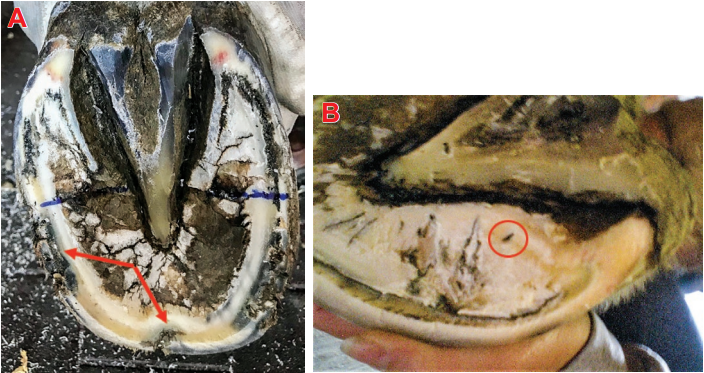 |
| Figure 1A&1B: Foreign debris will gain entry and accumulate in a small separation (red arrows) or fissure located in the sole-wall junction (white line) anywhere around the perimeter of the foot (A) including a fissure(circle)on the abaxial surface of the bars adjacent to the sole (B). |
Once the debris reaches the dermis inside the hoof capsule, the foreign material activates the animal’s immune system(defense mechanism) inciting an inflammatory response within the dermal tissue.The bacterium contained within the debris propagate, further accentuating the inflammatory response which draws inflammatory cells into the area. Enzymes released from the bacteria and from the invading inflammatory cells (white cells)lead to liquefaction tissue necrosis and the development of the grey/black exudate. The infection is quickly walled off with a thin layer of fibrous tissue to form an abscess.The inflammation and the pressure from the accumulation of the exudate exerted on the surrounding dermal tissue lead to the pain and clinical signs associated with a hoof abscess.
Clinical Signs
Most affected horses show a sudden onset of (acute) severe lameness. The degree of lameness varies from being subtle in the early stages to non-weight bearing. The digital pulse felt at the level of the fetlock is increased, usually bounding and the involved foot will be warmer than the opposite foot. With careful observation,unless the abscess is in the middle of the toe, the intensity of the digital pulse will be much stronger on the side of the foot where the infection is located. If the abscess is long standing, there may be soft tissue swelling in the pastern up to or even above the fetlock on the side of the limb corresponding to the side of the foot where the abscess is located. The site of pain can be localized to a small focal area through the careful use of hoof testers. Sometimes with acute lameness, the pain will be noted over the entire foot with hoof testers and,in this case, it is necessary to rule out laminitis,a severe bruise or even a possible fracture of the distal phalanx (P3).
 |
| Figure 2: When a tract or fissure is found, it can be followed within the sole-wall junction (white line) using a small thin loop knife, a 2 mm bonecurette or another suitable probe. A horseshoe nail makes an excellent tool for drainage. |
Treatment
There is still debate between the veterinary and farrier professions as to who should treat a hoof abscess and the best method in which to resolve the abscess. Considering that a walled off hoof abscess is an extension of the epidermis, it is the author’s opinion that the infection could be treated by either the veterinarian or the farrier. The most important aspect of treating a subsolar / submural hoof abscess is to establish drainage. The opening should be of sufficient size to allow drainage but not so extensive as to create further damage. When pain is localized to a small focal area with hoof testers, a small tract or fissure will commonly be found in the sole wall junction. The tract or point of entry may not always be visible as the sole wall junction is somewhat elastic and tracts in this area tend to close. In this case, a suitable poultice should be applied to the foot daily in an attempt to soften the affected area and eventually a tract will become obvious.
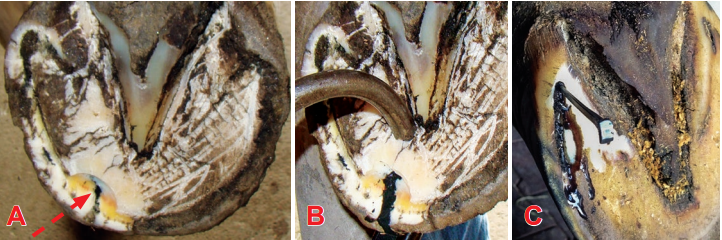 |
| Figure 3A, 3B & 3C: (A) red arrow shows approach to abscess through the sole wall junction. (B) shows the tract is open into the cavity of the abscess. A small opening is all that is necessary to obtain proper drainage. Pressure from hoof testers are used to promote drainage. (C) shows drainage at the heel using a horseshoe nail. |
When a tract or fissure is found, it can be followed / explored within the white line using a small thin loop knife, a 2 mm bonecurette or another suitable probe such asa horseshoe nail (Figure 2). The tract is slowly followed until a grey/black exudate(pus) is released and the probe enters the“belly” of the abscess. At this point, the tract is open into the cavity of the abscess.A small opening is all that is necessary to obtain proper drainage. This can be determined by using thumb pressure on the solar side of the tract just behind the opening or by placing hoof testers on the sole next to the tract and observing if more exudate is expressed or a bubble is forming at the opening of the tract when pressure is applied (Figure 3A & 3B). Care should be taken to avoid exposing any corium, as it will invariably prolapse through the opening, preventing closure of the tract and possibly creating an ongoing source of pain.Under no circumstances should a routine hoof abscess be approached through the sole!
The draining tract can be kept soft and drainage promoted in several ways. The author will generally apply a commercial medicated poultice a for the first 24-48 hours. The poultice is immersed in hot water, the water is squeezed out, the poultice is placed on the foot and attached with a roll of wide brown gauze, a cohesive bandage and waterproof tape (Figure 4a, 4b& 4c). The sheet version of this poultice is preferred rather than the poultice pad that is distributed by the company. The whole foot including the coronet should be enveloped in the poultice.
 |
| Figure 4: : Application of a medicated poultice. Submerge in hot water, squeeze out excess water, envelope the foot with the plastic side of the poultice on the outside. Secure to the foot with a wide brown gauze, cohesive bandage and duct tape. |
Another method to encourage drainage is to apply what is termed a ‘soak bandage’. Here layers of soft practical cotton (available in rolls) are folded together and then used to envelope the foot to form a thick bandage. MgSo4 (Epson Salts) is placed on the inner foot surface of the bandage and the bandage is attached to the foot as described above. The bandage is now saturated with hot water and then saturated periodically over the next 24-48 hours. Using either of these methods eliminates the necessity for continued foot soaking which can be cumbersome and possibly less effective.
Ichthammol ointment, which is a coal tar derivative with mild antiseptic properties,has been described for treating skin disease in both humans and animals. The use of an Ichthammol bandage for treating hoof abscesses, both before and after drainage,has become another traditional treatment used by veterinarians, farriers and horse owners with reportedly good results.However, the author has no experience using this product. There are numerous commercial products marketed to treat foot abscesses but these products will only be helpful if they complement the principles of drainage described above.
Once drainage is established the horse should show marked improvement within 24 hours. Once drainage has ceased, the hoof is kept bandaged with an appropriate antiseptic such as Betadine b solution/ointment or 2% iodine applied over the tract until the wound is dry and sealed. At this point, the opening of the tract is filled with a medicated hoof putty c which keeps the affected area clean and prevents further debris from entering the tract or wound.The shoe is replaced when the horse is completely sound.
 |
| Figure 5: Small channel created in the hoof wall with a small pair of half round nippers so tract can now be approached in a horizontal plane. |
Often, a painful tract can be located but drainage cannot be established at the sole wall junction. In this case, the infection is deep and may have migrated under the sole or wall away from the sole wall junction or white line. Again, under no circumstances should an opening be created in the adjacent sole! This seldom leads to the abscess and often leads to hemorrhage and may create a persistent, non-healing wound with increased potential for infection or osteomyelitis of the distal phalanx. Instead, a small channel can be created on the abaxial or hoof wall side of the sole wall junction using a small narrow pair of half-round nippers. The channel is made in a vertical direction following the tract to the point where it courses inward. Drainage can usually be established using a small probe in a horizontal plane (Figure 5).Preferably, this is done at an early stage of the lameness before the infection ruptures at the coronet.
If left untreated, a hoof abscess will follow the path of least resistance along the outer margin of the dermal tissue and eventually rupture at the coronet forming a draining tract. Many horse owners actually consider this to be an acceptable practice and elect to wait for this to take place.This practice often extends the time the animal experiences severe pain. Rupture at the coronet also leads to a permanent scar or tract under the hoof wall. This tract leading to the coronet may result in a prolonged recovery from the abscess, a chronic draining tract, repeated abscesses and a full thickness hoof wall crack. Every effort should be made to establish drainage of the abscess on the solar surface of the foot prior to a rupture at the coronet.
Infection from a misplaced horseshoe nail
Dermal tissue can be inoculated by bacteria from a misplaced nail in two ways. The nail can be driven directly into the laminar corium. When the nail enters dermal tissue,the horse will generally show discomfort as the nail is driven into the foot and there will be hemorrhage present where the nail exits the outer hoof wall. Blood observed at the exit of the offending nail will alert the farrier of the misplaced nail. The blood actually has a beneficial function as it acts as a “physiologic rinse” to dilute or eliminate bacterial contamination. Removal of the nail and application of an appropriate antiseptic will usually prevent infection.Another scenario that occurs frequently is while the farrier is driving a nail, the horse shows significant discomfort indicating the nail is invading dermal or sensitive tissue.Often the farrier will remove the nail, place it in another spot / direction and again drive it into the foot. However, when this scenario occurs, the farrier should remove the shoe and examine the spot where the nail entered the foot. If a nail has entered dermal tissue (even if removed), it causes trauma to the dermal tissue and can seed the area with organisms which may lead to abscess formation. If the nail has entered the foot inside the sole-wall junction, the owner/trainer should be alerted as to the potential problems and the horse can be placed on an oral broad-spectrum antibiotic for 3 – 5 days as a prophylactic measure. Lastly, we have the condition described as a “close nail” where the nail is placed such that it lies against the border of the dermis just axial to the hoof wall. Pressure against the corium combined with constant movement of the nail against the corium as the horse moves and bears weight may cause an inflammatory response and allow any bacteria that were introduced with the nail to form an abscess as described above.There is generally a lag period of 7-14 days or even longer before clinical symptoms or discomfort is observed following the placement of a “close nail”. Treatment again would be to establish and promote drainage.
Penetrating Injuries to the Foot
Puncture wounds to the solar surface of the foot most often occur when the horse steps on a sharp object(s) such as a fixed narrow solid object, a sharp rock, a nail or piece of glass which penetrates the horny sole. Superficial puncture wounds penetrate only the cornified tissue while deep wounds penetrate the germinal epithelium.Wounds to the sole need only penetrate 1 cm or less to invade germinal epithelium and seed the site with bacteria that leads to infection. Puncture wounds of the sole will be discussed here as puncture wounds that involve the soft tissue structures of the palmar / plantar foot are beyond the scope of this article.
Farriers are often asked to treat puncture wounds to the solar surface of the foot.Medications such as antibiotics and anti-inflammatory drugs may be indicated and will need a veterinarian’s prescription. If a farrier were to treat an established infection in the hoof, it would be perceived as practicing veterinary medicine and the farrier could be held liable. Farriers are often asked to place a shoe with a removable treatment plate on the foot with a puncture wound for protection but at the same time allowing access for daily treatment.As drainage ceases and the puncture wound begins to cornify, the farrier will be asked to place a pad between the hoof and shoe for protection until healing is complete.
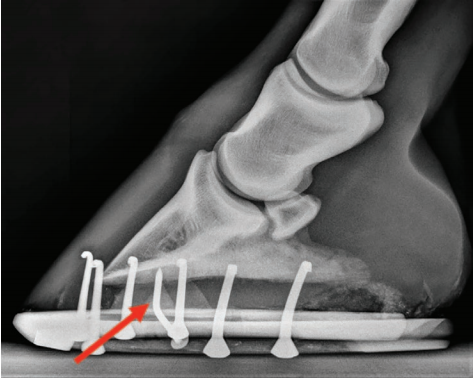 |
| Figure 6: Small channel created in the hoof wall with a small pair of half round nippers so tract can now be approached in a horizontal plane. |
Clinical Presentation and Diagnosis
Puncture wounds frequently create marked lameness. The degree of lameness may vary considerably depending on the depth, location and duration of the wound. Superficial wounds may initially have minimal lameness but can progress to severe lameness within several days with the development of an infection. In general, puncture wounds that invade the corium become quite painful soon after the injury as the corium above the horny sole seals, thus preventing any further drainag eand creating a medium for infection.Progression to severe non-weight bearing lameness can occur as the rigid hoof capsule restricts the swelling associated with not only the inflammatory response from the trauma of the puncture wound but the resultant infection within the dermis.Wounds that involve damage to deeper structures such as the distal phalanx (fracture)are painful from the onset. Depth of penetration can be difficult to ascertain when the wound progressives past the horny sole and the severity of the clinical signs do little to help define which structures are involved. An increased digital pulse is common and, in some cases, the digital pulse may be increased only on the affected side (often with a recent wound). Increased heat may be palpable at the coronary band and/or over the hoof capsule in the affected limb. Longstanding wounds may lead to a diffuse swelling in the soft tissue of the pastern and above. Early hoof tester application after the injury may reveal focal sensitivity but over time a painful reaction may be elicited over the entire sole region.Visual inspection of the solar surface of the foot may reveal the source of the lameness but often the defect in the sole is not apparent. If the offending object such as a nail is noted, an attempt to obtain a radiograph is essential in order to measure the direction and depth of penetration and to evaluate which structures may be involved (Figure 6). Examination should begin by cleaning the solar surface of the foot with a wire brush and paring the sole lightly with a hoof knife; this may reveal the site of the puncture wound, a black tractor a crack in the horny sole. Due to the invasive nature and serious complications that can occur following puncture wounds,it is the author’s opinion that when dermal tissue is involved and requires debridement,a veterinarian should become involved in the case. Any delay in the initiation of the appropriate treatment can have serious consequences.Debridement may be painful and necessitates the use of local analgesia at the level of the palmar digital or abaxial sesamoid nerves. Once the surface of the foot is cleaned and the wound or tract is identified, a sterile prep of the foot with an antiseptic scrub and alcohol rinse should be performed. This will allow further exploration of the wound without fear of contaminating the surrounding normal tissue. Probing the wound with a blunt sterile probe or teat canula can help determine the depth and direction of the wound tract.Radiographs taken with the probe or canula in place is another option to accurately assess depth and direction of the wound along with any gas shadows, debris or any radio-opaque foreign bodies that may be present. If an obvious crack or black tract is found, exploration may lead to a pocket of infection and subsequent drainage. A small looped hoof knife or a bone curette (# 2) is useful to explore these areas.
Penetrating objects are contaminated with dirt, rust and manure and this material may be driven deep into the wound. Without adequate drainage an anaerobic environment develops that promotes the growth of anaerobic bacteria. Contamination with the organism Clostridium tetani is of particular concern because of the potential threat of tetanus. This disease is difficult to treat successfully and an inquiry into the animal’s history of appropriate vaccination is important. Although adequate immune protection may exist from a previous vaccination with tetanus toxoid, a booster of tetanus toxoid should be given in the event of a puncture wound to the foot. Superficial wounds carry a good prognosis and can have dramatic resolution of lameness within 24-48 hours following drainage while deeper wounds require surgical debridement. Superficial wounds and infections are effectively treated by establishing drainage, applying an antiseptic bandage until drainage has ceased and protecting the foot until the hoof capsule defect has healed.
Long standing and deeper puncture wounds require more extensive debridement.Surgical drainage and debridement of necrotic soft tissue or possibly infected bone is necessary for the wound to heal.Wounds to the sole can be safely explored and debrided with the horse standing using local analgesia. The horse should be placed on systemic antibiotics and anti-inflammatory medication before surgery. An area of sole 1–2 cm in diameter should be removed around the puncture site in a conical fashion so that the tract can be completely explored. The surgical approach should follow the draining tract and allow adequate exposure for removal of any diseased tissue and to establish sufficient drainage.Creating the wound in a conical manner prevents the corium from prolapsing into the drainages site which is both painful and prevents healing.
REFERENCES